Eyelid Malpositions
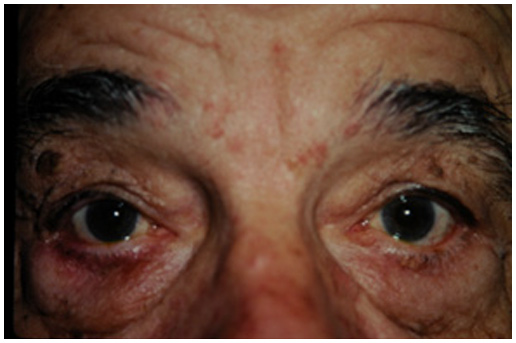
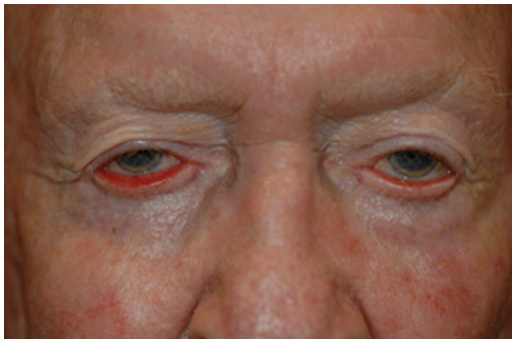
If you have ever felt an eyelash in your eye, you can imagine how irritating it would be to have an inward turning eyelid. The constant rub of lashes against your eye is not only irritating, but can lead to a serious, visually threatening infection. Similarly, an outward turning eyelid may result in tearing, redness, mattering and irritation. An outward turning eyelid may cause permanent damage from exposure of the eyeball, occlusion of the tear duct and scarring. In some cases, the eyelid may be both flipped out (ectropion) and curled in (entropion) at the same time! Additionally, eyelids may become peaked, retracted or develop contour abnormalities that prevent them from acting as a “windshield wiper.” In each of these circumstances, the eyelids cannot perform their normal job of protecting the eyeball, maintaining a normal tear film and draining tears.,
Eyelid malpositions are the result of forces acting upon the eyelid margin. A normal eyelid should have a quick return snap to the eyeball. Frequently, tendon laxity at the inner and outer corners (canthi) of the eyelid will render the eyelid margin unstable making it susceptible to contractile forces. For example, when a facial scar near the lower eyelid contracts, it may pull a lax lower eyelid away from the eyeball. In addition to canthal support, the eyelids are supported by “retractors” that open the eyelids. The retractors are tendon extensions of the vertical muscles surrounding the eyeball. Thus, when you look up or downward, the eyelids follow your gaze. When the retractors are pathologically altered, eyelid malpositions may include retraction (stare), entropion (inward turning), and contour peaks or troughs.
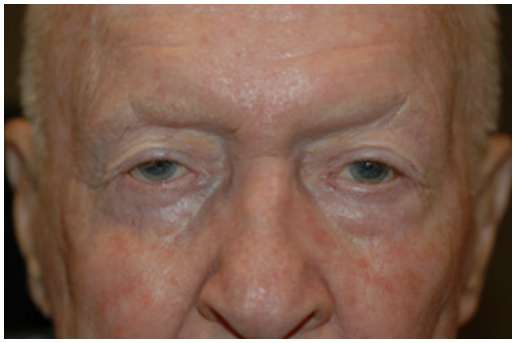
The goal in treating a given eyelid malposition is to reposition the eyelid so that the new healing forces will overcome the pathologic forces. In eyelid repair as in “Star Wars” the phrase “May the force be with you” applies. The surgery to reposition an eyelid varies with the underlying cause of the eyelid malposition. The common approaches include eyelid and canthal tendon tightening, eyelid retractor advancement or recession and skin grafting or transposition flaps.
This type of surgery is typically performed on an outpatient basis under local anesthesia, with sedation. The amount of post-operative swelling may vary depending upon a variety of factors, but typically resolves after two weeks. A small amount of swelling/black and blue may persist for as long as six weeks following surgery. The use of ice compresses within the first 48-72 hours of surgery will significantly reduce swelling and promote a more rapid recovery.
There are normally three post-operative visits; the day after surgery to check your vision, the week after surgery to take out sutures and the month after surgery to take final photos.